I. Indications
A. Inability to obtain peripheral IV access.B. Need for specific IV medications that may be caustic to peripheral veins (D25,
pressors, hypertonic saline).
C. Transvenous pacing.
D. Central venous pressure monitoring.
ENeed for emergent dialysis without previous access
II. Contraindications
A. Peripheral access obtainable without other indication for central access.B. Cellulitis or anatomic abnormality.
C. Coagulopathy is an absolute contraindication to subclavian cannulation, as it is a
non-compressible site and a relative contraindication to the internal jugular and
femoral sites.
III. Equipment
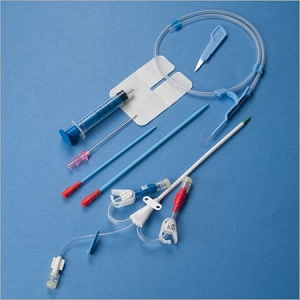
A. Most of the equipment needed to perform central venous cannulation can befound in commercially available central line kits . Kits include
povidone-iodine (Betadine) swabs, guidewire introducer needle, J-tip guidewire,
multiple 5-mL syringes, 1% lidocaine, 22- and 25-gauge needles for local anesthe sia, #11 blade scalpel, dilator, central line, and silk suture on a straight cutting
needle.
B. There are multiple types of central lines. Generally, 1 of 2 types is used in the ED
(Figure 3–2). A triple lumen catheter is used in patients when there is difficult
IV access or those who require multiple different medication drips. A sheath in troducer (Cordis®) catheter is shorter and wider and is used for the introduc tion of Swan-Ganz catheters, transvenous pacers, and for rapid infusion of fluid
and blood products in the hypotensive patient. These larger catheters can achieve
flow rates up to 1 L/min.
IV. Procedure
A. Preparation. Locate anatomical landmarks. Apply povidone-iodine to the area ofneedle insertion. Place sterile drape with fenestration over the area. Anesthetize
with lidocaine.
B. Seldinger Technique
1. Use large bore needle with syringe to cannulate the vein. There should be free
flow of dark non-pulsatile blood into the syringe with traction on plunger
2. Thread the guidewire through the needle until 3–5 cm of the guidewire re mains If resistance is met, withdraw the wire and confirm that
the needle is in the vessel. Attempt to rethread the wire.
3. When the guidewire is in place, remove the needle (. Never let go
of the guidewire during any part of the procedure because it can migrate
fully into the vessel.
4. Using a #11 blade scalpel, make a superficial stab incision in the skin at the site
that the guidewire enters
5. Pass the dilator over the wire and thread into the vessel . (For the
Cordis® catheter, the dilator and catheter are inserted together.)
6. Remove the dilator and thread the triple lumen over the wire until it protrudes
2–3 cm out of the brown port.
7. Holding the wire with one hand, thread the line into the vein
8. Remove the wire and confirm placement with aspiration of blood
. Secure the catheter in place with suture.
C. Internal jugular vein . Position the patient supine and in slight
Trendelenburg position. Rotate the head 75° to the opposite side. Palpate the tri angle formed by the 2 heads of the sternocleidomastoid muscle. Palpate the
carotid artery pulse within this triangle. The vein is lateral to the artery in this lo cation. Ultrasound is frequently used to help identify the vein. Insert the needle at
the apex of the triangle, aiming toward the ipsilateral nipple with 30° of angula tion. The vein should be entered within 2–3 cm of needle advancement.
Place a rolled sheet or towel between the patient’s scapulas to allow the
 shoulders to fall backward and flatten the clavicles. Insert the needle 1 cm inferior to the clavicle, aiming towards the junction of the middle and medial thirds. Direct the needle under the clavicle and toward the suprasternal notch, with the needle parallel to the chest wall. The vein should be entered within 4 cm of needle advancement.
shoulders to fall backward and flatten the clavicles. Insert the needle 1 cm inferior to the clavicle, aiming towards the junction of the middle and medial thirds. Direct the needle under the clavicle and toward the suprasternal notch, with the needle parallel to the chest wall. The vein should be entered within 4 cm of needle advancement.
E. Femoral vein Palpate the femoral artery 2 cm below the inguinal crease. The vein is usually 1 cm medial to the artery at this location. Insert the
needle at a 45° angle to the skin, medial to the femoral pulse. In the pulseless pa tient, palpate thanterior superior iliac spine and the pubic tubercle. Draw an
imaginary line connecting these 2 points. If this line is divided into thirds, the
vein will be located where the medial and middle thirds intersect.
V. Complications:
A. Internal jugular vein. Bleeding, airway compression from expanding hematoma,
carotid artery dissection, pneumothorax, air embolism, or arrhythmia from car diac irritation .
B. Subclavian vein. Bleeding, pneumothorax, air embolism, or arrhythmia from car diac irritation.
C. Femoral vein. Bleeding, DVT of femoral vein, femoral artery laceration, soft tis sue infection, or line sepsis.
SOURCE USMLE

0 التعليقات:
Post a Comment